What is Endometriosis?
The normal endometrium
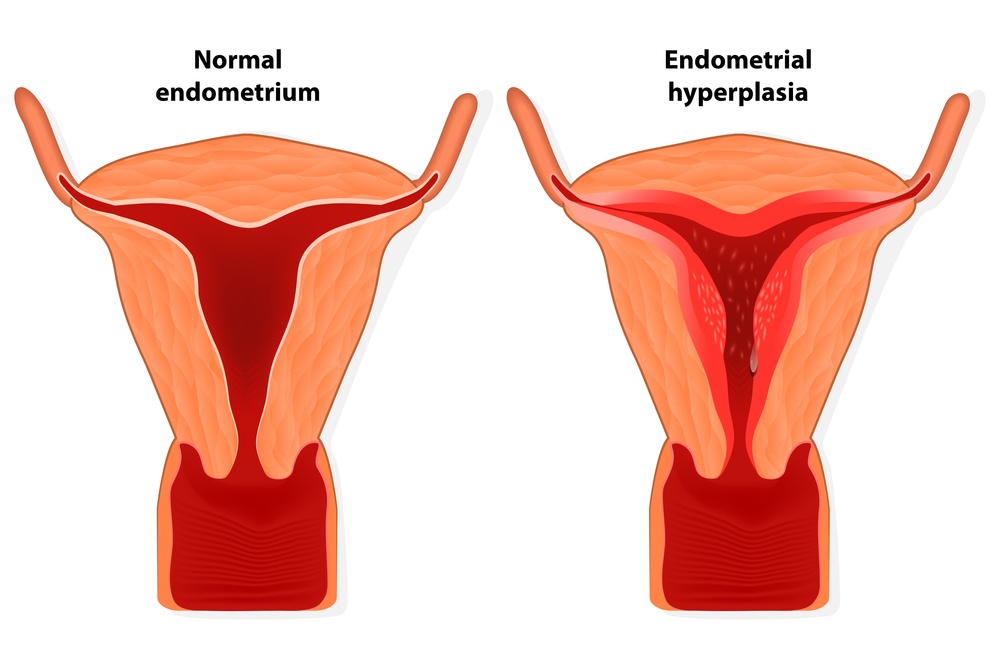
Endometriosis takes its name from the lining of the womb, which is called the endometrium. The endometrium forms the uterine lining in which the early embryo implants. It is the most dynamic of all tissue in the body, as it is shed each month and then completely regrows.
At the beginning of the female monthly cycle the endometrium responds mainly to oestrogen and rapidly proliferates, thickens and becomes receptive for embryo implantation. The endometrium is maintained in this state by progesterone in the second half of the cycle. If pregnancy does not occur, progesterone levels fall and the endometrium disintegrates and bleeding occurs, and then the cycle begins again.
Displaced endometrial tissue in the pelvis
The problem of endometriosis arises when some areas of endometrial tissue appear outside of the womb and a found somewhere else in the pelvic cavity. Once established these areas of endometrial tissue continue to respond to female hormones as if they were lining the womb. That is to say, they grow during the first half of the cycle and break down and are shed into the pelvic cavity at the end of the cycle.
Unlike menstrual fluid from the uterus, which is discharged from the body during menstruation, blood from the misplaced endometrial tissue remains in the pelvis and may cause inflammation surrounding the area. Inflammation can produce scar tissue around the area of endometriosis. These endometrial tissue sites may develop into permanent lesions or patches of endometrial tissue leading to scar tissue or cysts.
Mild forms of endometriosis are common and may not require treatment. Severe or chronic endometriosis can make it difficult for a woman to become pregnant.
What Causes Endometriosis?
The precise causes of endometriosis are not known and are still the subject of scientific debate. However, the most widely accepted view is that tiny fragments of endometrium travel through the fallopian tubes and escape into the pelvic cavity. The endometrial tissue then implants onto the surface of uterus, ovary, bladder, bowel, fallopian tube or some other pelvic site, where it continue to grow and respond to female hormones as if it were still lining the womb, bleeding each month at the time of menstruation. Overall the disease affects between 5-10% of all women.
Symptoms
Endometriotic lesions vary considerably in size, from the size of a pinhead to large clumps many centimetres across. In many women there are no symptoms and the disease may go undetected. Overall, the larger and more extensive the patches of endometriosis, the worse the symptoms, but this is not always the case.
When symptoms are present, they may include :
Abdominal cramps.
Back pain during menstruation.
Painful bowel movements or urination during your period.
Painful sex.
Difficulty in becoming pregnant.
How Endometriosis Can Affect Fertility
Around 30-40% of women with endometriosis experience fertility problems, which is two or three times the rate of infertility in the general population. The chance of becoming pregnant decreases by approximately 10-30% in women with endometriosis. However, women with mild cases of endometriosis are affected less than those with severe endometriosis. The site and nature of the endometriosis is also a factor in determining the effect on fertility.
Scar tissue resulting from endometriotic lesions can block the fallopian tubes or interfere with ovulation. Patches of endometriosis can to be sticky, for example a section of bowel or area of the bladder may stick to outer surface of the uterus and these are called adhesions. In severe cases, ovarian cysts called endometrioma sometimes form and these also interfere with ovulation.
It is thought that some of the products of inflammation such as prostaglandins may interfere with the functioning of the fallopian tube and the normal passage of the egg along it. Similarly, production of inflammatory cytokines may affect sperm motility or implantation of the developing embryo in the womb.
Diagnosing Endometriosis
There is currently no reliable blood test for endometriosis. The endometriotic lesions may be very small, and while they can sometimes be seen using ultrasound or magnetic resonance imaging (MRI) this is often not the case and a normal appearance in these tests does not guarantee that endometriosis is absent. Because of these considerations the only truly reliable method for diagnosis is laparoscopy.
Laparoscopy involves making a small cut in the abdominal wall below the umbilicus (belly button) under anaesthetic. A laparoscope (a thin fibre optic tube containing a camera) is passed through and the doctor can clearly see whether patches of endometriosis are present.
Estimating the Deverity of Sisease (Staging)
The severity of endometriosis is recorded according to complex staging criteria which assesses the lesions, their locations and any adhesions in the pelvic cavity. The main uses for staging are in following the progress of endometriosis and at least knowing whether it is improving or getting worse. Further, staging allows standards in the severity of the disease to be set and these are then used to compare clinical situations in the various studies worldwide.
Unfortunately, the results so far indicate that there is often little or no relationship between the severity of endometriosis and its symptoms, so that a woman with severe disease may have fewer symptoms than one with minimal disease. The location of the endometriosis can give some indication of any likely effect on fertility, for example, blockage of fallopian tubes of heavy involvement with the ovary, but even then the stage of disease may not correlate with fertility.
Stage I (Minimal) – Small superficial lesions or a few light adhesions.
Stage II (Mild) – As stage I, but some deep lesions present.
Stage III (Moderate) – As stage II, plus presence of endometriomas on the ovary and more adhesions.
Stage IV (Severe) – As stage II, plus extensive adhesions or large endometriomas.
If endometriosis not treated it tends to get worse in around 40% of cases. The situation improves in around 30% of cases and there is no appreciable change in the remaining 30%. However, severe untreated endometriosis can occasionally cause more serious complications such as kidney or bowel problems. Large endometriomas (greater than 2cm) are removed surgically to prevent them rupturing and bleeding excessively.
Treatment of Endometriosis
Most treatment for endometriosis is geared towards managing symptoms rather than altering the pathology of the disease. Many women with mild symptoms simply rely on painkillers such as paracetamol or ibuprofen. In addition to this there are some hormonal treatments which may ease pain associated with endometriosis.
Hormone treatments for endometriosis generally rely on the fact that endometrial tissue grows in response to oestrogen. They work by reducing the amount of oestrogen in the body or by blocking the effect of oestrogen on the endometrial cells. These include the concraceptive pill, gonadotrophin releasing hormone (GnRH) and progestogens. Hormonal or medical treatments are ususally continued for at least 6 months before reassessment. All of these treatments have their own applications, but none of them are useful in preserving fertility during the actual treatment, so this can mean at least a six month wait before trying for a baby.
Fertility preserving treatment
Just as laparoscopy is the gold standard in the diagnosis and staging of endometriosis, then laparoscopic surgical removal or ablation of the endometriotic lesions using lazers or applied heat is the often treatment of choice for fertility preservation in endometriosis. Sometimes diagnosis and treatment are carried out at the same time in a single laparoscopic procedure. The specialist may ask for consent to treat any large endometrial lesions that they find whilst they are performing a diagnostic laparoscopy.
Assisted reproduction techniques (ART)
Assisted reproduction procedures can increase the chances of pregnancy even in women with untreated endometriosis. In IVF treatment ovulation is bypassed as eggs are collected surgically. In addition, both fertilisation and early embryo development occur in the laboratory rather than in the fallopian tubes or uterus, and so avoid the problems of blocked tubes or an inflammatory environment in the pelvis. Sometimes, surgical treatment of endometriosis is combined with IVF gives good results. Each case is unique and so you should consult your physician about the best strategy for dealing with endometriosis. The symptoms of endometriosis usually lessen during pregnancy. Whatever the type of treatment, it should be remembered that endometriosis may recur in the future. Symptoms usually subside and may disappear after the menopause.
Science Director Concept Fertility Clinic www.conceptfertility.com