Why produce embryos at all?
Embryos are produced in In-Vitro Fertilisation (IVF) laboratories from eggs and sperm and are transplanted into the wombs (uterus’s) of their mothers a few days later. Most embryos, whether produced naturally or through IVF, fail to develop and this is why multiple embryos are produced in the IVF process – if the chances are, say, that only 1 in 6 embryos will develop into a viable baby, it is better to have 6 embryos developing in the laboratory at the start of the process rather than having 6 separate cycles of IVF, each with a single embryo.
The naturally high rate of embryo failure is also the reason why people do not achieve successful pregnancies every month they try and why couples often do not announce their pregnancy until after the first 3 months have passed. Further, it is the reason why doctors usually tell patients to try to get pregnant naturally for several months before they consider fertility treatment.
Another important reason for producing embryos in a laboratory is for research, to continue the trend of improvements in IVF success rates, and this is where the current debate on extending the time limit for growing embryos is relevant. When IVF was first tried, its success rate was zero. The parents of the world’s first IVF baby, born in 1978 were told that their chances of success were one in a million. But they got lucky and had that baby! Over the years techniques have developed and improved, and the number of IVF babies in the world is now estimated to be approaching six million. However, the most recent UK national figures (for 2013) still only show a success rate of about 25% for all IVF cycles started, for all patient ages. The vitrifying technique for cryogenically freezing embryos has developed at the same time so that now, if any surplus embryos are produced, they can be frozen and transferred back to the mother later in a process that is much simpler than another full cycle of IVF.
What is the legal position?
IVF clinics and research laboratories in the UK are highly regulated by the health authorities and the law states that embryo research cannot be carried out beyond 14 days. Until recently that was almost irrelevant because scientists could not keep embryos alive outside the body for this long anyway. However, researchers in Cambridge recently developed techniques which kept embryos alive in their laboratory for 13 days and it is assumed that they could have been kept alive for longer if it had not been for the 14-day rule. Many prominent scientists, and even some religious leaders, have argued that to allow research to continue, the 14 day limit should be extended to 28 days. The health authorities have currently said that the limit will not be extended but scientists have continued to argue for the benefits of an extension.
How is the time limit for keeping embryos set?
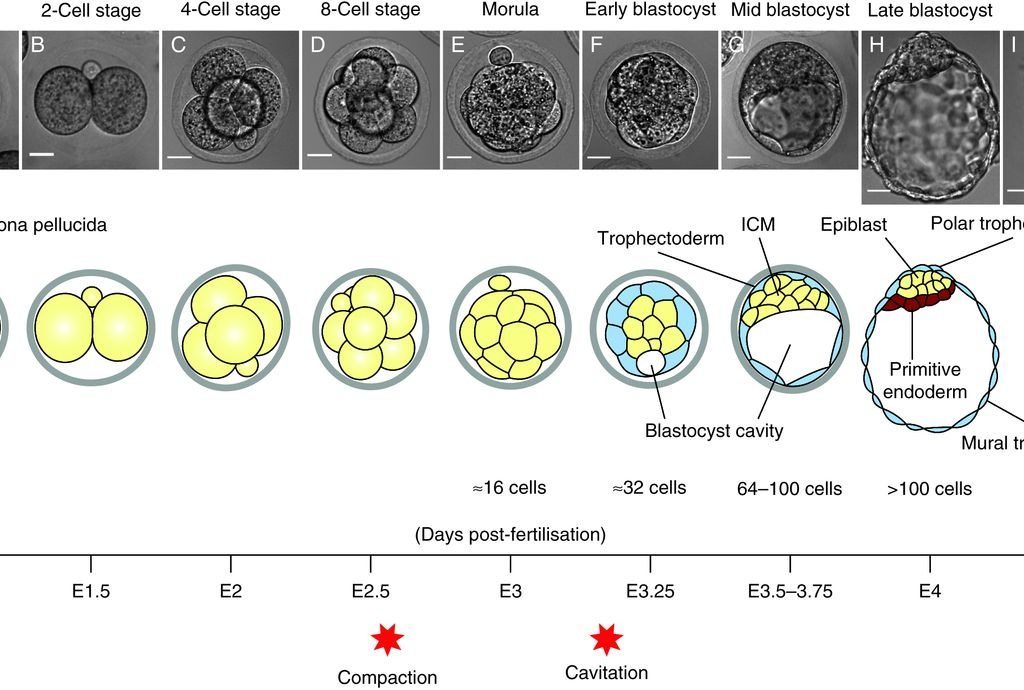
Back in 1984 Baroness Warnock suggested that 14 days should be the limit as this is the point at which an embryo’s individuality could be asserted and it can no longer split to become identical twins. This was enshrined into law with the HFEA Act of 1990. Others have pointed out that the first stages of nerve development happen around day 17. Practically, when IVF clinics treat patients, the limit is not much more than 5 days. This reflects the period of time in nature where the egg/embryo remains unattached in the fallopian tube before it moves into the uterus and starts to implant. Unless this connection to the uterus starts on time, the embryos perish. The new research in Cambridge has developed methods which chemically mimic the presence of the endometrial lining of the uterus and allow the embryo to survive in the laboratory through the time period when it would normally be implanting in the womb.
Why extend the research period to 28 days?
Studying gastrulation, the period where the embryo is between 7 and 28 days old, is argued to be critical for understanding how human cells develop and promises major insights into congenital conditions, heart disease and cancers. It would allow scientists to investigate the causes of early miscarriages and study the points in time when there are the greatest number of implantation-related pregnancy failures. If this eventually leads to a reduction in the number of miscarriages it can only be a good thing.
What’s next?
Currently the law stands at a 14 day limit for embryo research. The Cambridge research will allow doctors and scientists to better study what happens between days 7 and 14 and this could lead to huge improvements in medical techniques. Studying what happens between days 14 and 28 would almost certainly lead to further improvements but it is absolutely essential that such decisions are taken carefully and with informed public debate. Expect to read more about this in news headlines in the coming months and years.